Elisabeth Morgans, Senior project manager at C3 Collaborating for Health, discusses solutions to tackle physical inactivity and overcome the ever pervasive and entrenched issue of health inequality
According to the UK government, adults should accumulate at least 150 minutes (two and a half hours) of moderate intensity physical activity or 75 minutes of vigorous intensity activity every week. (1) Yet in 2020/21, almost 30% of adults in England participated in less than 30 minutes of physical activity per week, sadly meeting the criteria to be labelled as ‘physically inactive.’ (2)
Physical inactivity is in itself a pandemic – and a leading cause of death globally. (3) According to the World Health Organization over a quarter of the global adult population (1.4 billion adults) is insufficiently active, and there have been no improvements in global levels of physical activity since 2001. (4) In fact, in high-income countries, (which boast inactivity levels twice as high as those observed in low-income countries), insufficient activity increased by 5% between 2001 and 2016.(4)
Why is physical inactivity an immense problem?
The undisputed benefits of physical activity on physical and mental health are well documented, and subsequently, physical activity is a key pillar of all chronic disease prevention strategies worldwide, in addition to the other risk factors such as smoking, diet and alcohol. The evidence for physical activity is compelling – inactivity is associated with one in six deaths in the UK and up to 40% of many long-term conditions, including preventable conditions such as type 2 diabetes, cardiovascular disease and some cancers. (5)
Furthermore, physical activity – in its simplest form – is completely free. Whilst some can’t resist the lure of muscle building machinery in a gym or the purchasing of hi-tech sportswear and expensive gadgets, a brisk walk outdoors or a bike ride to work, gardening or housework, offer an undeniable economic advantage compared to expensive gym memberships and costly sportswear.
So why is it that almost a third of England’s adults, and a quarter of the global population, are failing to meet weekly physical activity guidelines? The answer is complex and nuanced, but essentially lies in the ever pervasive and entrenched issue of health inequality.
Common tropes and soundbites used by the media, the health and wellness industry, health bodies and authorities aim to promote the simplicity of individual behaviour change to enable more physical activity. They include getting off the bus one stop earlier, walking in nature, taking public transport, or walking instead of driving. These options are frequently appointed descriptions such as ‘simple steps’ or similar descriptors that reinforce the ease of participating in daily physical activity.
Furthermore, I can state with confidence as a physiotherapist that health professionals routinely prescribe and promote physical activity for patients as part of a rehabilitation programme, yet all too frequently do not consider the environments in which people live – and fail to recognise the immense influence that our environment has on our daily choices and ability to easily choose the healthier option.
The link between health inequality and income inequality
What if there are no green spaces nearby to walk or run? What if you don’t feel safe being outdoors alone? What if public transport links are absent or unreliable? These environmental factors have a huge impact on physical activity participation. Where we live influences how we live – and how active we are. Consider pavements, bike lanes, cars, safe crossings, and local amenities within walking distance such as parks, shops, access to green space, fast food, fresh food, social connectedness – all these factors influence health.
All too often, the focus is on convincing individuals to change unhealthy behaviours that are contributing to their risk of non-communicable diseases (NCDs). This is particularly true for disadvantaged communities, where healthy food options and opportunities for physical activity may be non-existent or unrealistic. It is well established that a social gradient exists with respect to health, which was well documented by Sir Michael Marmot over a decade ago – the lower a person’s social position, the worse their health; (6) in both high-income countries and low-income countries a lack of physical activity is strongly associated with income inequality.(7)
According to Sport England, the COVID-19 pandemic has widened existing inequalities in physical activity, which have significantly affected women, young people, the over 75’s, disabled people and people with long-term health conditions, and those from Black, Asian and other minority ethnic backgrounds, and those individuals living in deprived and urban areas, who have found it harder to be active. (2) These findings chime with earlier research conducted in the U.S. by Moore et al (2008) who evidenced that facilities and resources conducive to physical activity are not equitably distributed. Minority neighbourhoods are significantly more likely than white neighbourhoods to lack recreational facilities and deprived areas are more likely to lack facilities compared to high-income areas.(8)
Creating an environment conducive to physical activity is just one way to approach the non-communicable disease epidemic. Putting communities – who are the experts in their own health needs and their environment – at the heart of decision making through a whole systems approach aims to identify barriers to good health and use a community’s existing strengths to overcome these barriers. The aim is to make the healthy option the easy option for all to create sustainable change. The World Health Organization agrees. Its Global Action Plan on NCDs 2013-2020 stresses that ‘empowerment of people and communities’ is essential in addressing the NCD epidemic.(9)
C3 Collaborating for Health
At C3 Collaborating for Health (C3), we seek to prevent NCDs by promoting three behaviour changes:
- Improving diet.
- Increasing physical activity.
- Stopping smoking.
Through multi-sector collaboration, we work with communities to make it easier for everyone to make healthier choices, which we know is especially difficult for those living in disadvantaged communities.
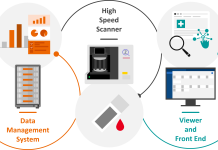
At the heart of C3’s community engagement strategy sits CHESS (Community Health Engagement Survey Solutions). CHESS is an innovative, evidence-based approach that shifts decision-making to local communities by engaging them as ‘citizen scientists’ in a systematic investigation about their health and the built environment (e.g., the shops, restaurants and parks in their neighbourhood).
CHESS uses a mobile application that surveys the built environment and equips local communities to identify and map the barriers they face every day when making choices about diet, activity and healthy living.
ASPIRE
C3 is currently working with seven communities in the North of France and the South of England via an EU-funded project ASPIRE (Adding to Social capital and individual Potential In disadvantaged Regions). This multi-partner project aims to address the complex issues of obesity and unemployment.
References
- Dept of Health & Social Care. UK Chief Medical Officers’ Physical Activity Guidelines.; 2019.
- Sport England. Active Lives Adult Survey May 2020-21 Report.; 2021. Accessed January 10, 2022. https://sportengland-production-files.s3.eu-west-2.amazonaws.com/s3fs-public/2021-10/Active%20Lives%20Adult%20Survey%20May%202020-21%20Report.pdf?VersionId=YcsnWYZSKx4n12TH0cKpY392hBkRdA8N
- Kohl HW, Craig CL, Lambert EV, et al. The pandemic of physical inactivity: Global action for public health. The Lancet. 2012;380(9838):294-305. doi:10.1016/S0140-6736(12)60898-8
- World Health Organisation. Physical Activity. Published November 26, 2020. Accessed January 6, 2022. https://www.who.int/news-room/fact-sheets/detail/physical-activity.
- Public Health England. Health Matters: Physical Activity Prevention and management of long-term conditions. Published January 2021. Accessed January 10, 2022. Health Matters: Physical Activity Prevention and management of long-term conditions. Health inequality.
- Marmot M. Fair Society, Healthy Lives the Marmot Review.; 2010. Accessed January 10, 2022. https://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review/fair-society-healthy-lives-full-report-pdf.pdf.
- Sfm C, van Cauwenberg J, Maenhout L, Cardon G, Lambert E v., van Dyck D. Inequality in physical activity, global trends by income inequality and gender in adults. International Journal of Behavioral Nutrition and Physical Activity. 2020;17(1). doi:10.1186/s12966-020-01039-x.
- Moore L v, Roux AVD, Evenson KR, Mcginn AP, Brines SJ. Availability of Recreational Resources in Minority and Low Socioeconomic Status Areas. Published online 2008:16-22.
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases, 2013-2020.; 2013. Accessed January 10, 2022. https://www.who.int/publications/i/item/9789241506236
Please note: This is a commercial profile
© 2019. This work is licensed under CC-BY-NC-ND.