Andrew Metcalfe, Director of Intelligent Infection Control Services Limited, LumiBio, explores the lessons learned in infection prevention and control
Professor Jonathan-Van-Tam (Deputy Chief Medical Officer for England) recently wrote in The Lancet “it is critical to use the lessons learned so far in the pandemic to minimise the burden of hospital-acquired infections, and to consider new approaches to reduce the burden further.” And then went on to recommend “robust hospital infection prevention and control policies that include staff vaccination, environmental disinfection, and appropriate isolation”. (1)
But should it take a global pandemic to highlight problems with Hospital Acquired Infections (HAI) and look to learn lessons in infection control? It isn’t as though there wasn’t a problem pre-covid, but perhaps it didn’t grab attention like it should.
The pandemic will skew recent figures, so we’ll go a little further back and look at the situation in the ‘old normal’.
“More than four million people in Europe acquire a healthcare-associated infection (HAI) every year, of whom approximately 37,000 die as a direct result of the infection. The death toll from HAI is comparable to the number of people who die each year in road traffic accidents.” (2)
Fatal road traffic accidents often make the local news, sometimes national, but hospital deaths from acquired infection… As it is, these figures are at the lower end of estimates. The World Health Organisation estimates 50,000 deaths in Europe from HAI, but at least 135,000 cases where HAI contributed to death.(3)
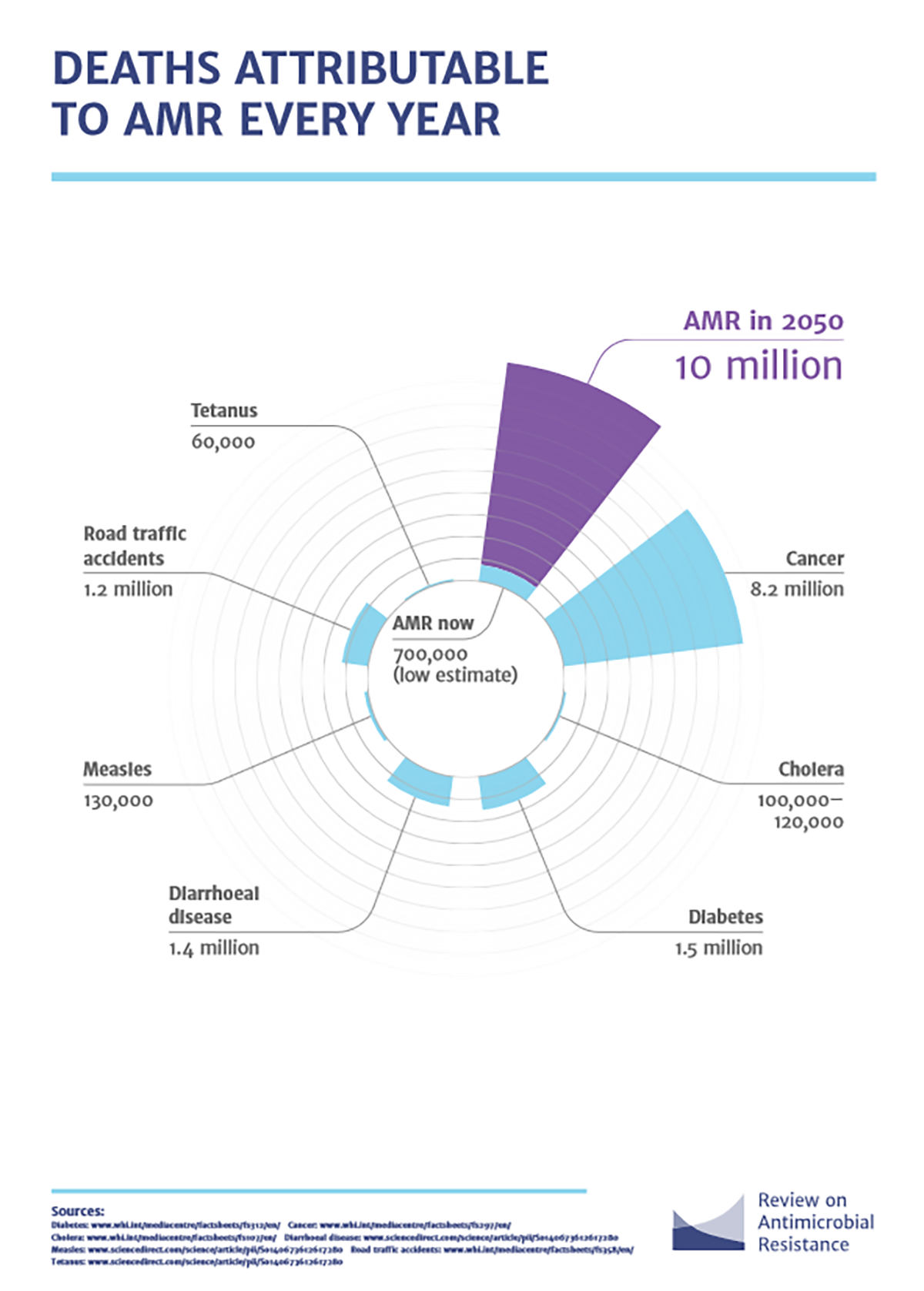
There has been little if any changes in infection control procedures for years. The previous strategy of using drugs has been found wanting and there are now active measures to reduce use of antimicrobials. Unfortunately, we were a bit late to the party and antimicrobial resistance (AMR) is now a huge issue in healthcare. (4)
The cost of lives isn’t the only issue. With the NHS overstretched and under resourced, the cost of HAI in beds and staff needs to be acknowledged.
In 2016/17 21% of all bed days across NHS hospitals in England and 79,700 days of absenteeism among front-line Healthcare Professionals were attributed to HAI’s.(5)
The financial cost runs into £billions.
The NHS National Standards of Healthcare Cleanliness 2021 recognise the importance of auditing cleaning procedures and the use of measurement/evaluation systems, although not mandatory and still only a visual check is required.(6)
So, what to do?
To quote Professor Van-Tam: “use lessons learned” – existing procedures aren’t good enough.
“consider new approaches” – be receptive to emerging technologies and new ideas.
“policies that include…environmental disinfection” – minimise the risk of infection from pathogens in the built environment.
LumiBio has been providing a cost effective, auditable infection control service in healthcare settings that meets the requirements for the pandemic and beyond.
LumiBio has demonstrated, in all circumstances, and beyond doubt, the ability to dramatically reduce pathogen levels, in working environments, to zero or close to zero.
Areas that were subject to traditional cleaning methods only, consistently recorded more occurrences of pathogen spikes and higher pathogen levels which as a result present a higher level of infection risk and infection transfer risk, to staff, patients and building users.
This provides a hugely significant advancement of clinical environmental standards.
LumiBio has achieved these exceptional results without any interruption to services, and without placing any additional burden on staff.
Integration of LumiBio is assisting IPC leads and FM teams to meet achieve regulatory compliance, providing fully auditable data and minimising the risk of infection to both staff and patients alike.
By embracing fully evidenced systems such as this, the NHS can provide a safer environment and reduce infections and deaths. This would lead to the commensurate savings in bed use, staff absence and financial costs.
It may have taken a global pandemic, but finally, are we going to ‘use the lessons learned’?
References
(1) Hospital-acquired SARS-CoV-2 infection in the UK’s first COVID-19 pandemic wave. The Lancet August 12, 2021, https://doi.org/10.1016/S0140-6736(21)01786-4
(2) Point prevalence survey of healthcare-associated infections, antimicrobial use and antimicrobial stewardship in England Protocol, 2016. Public Health England https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/773832/PPS_Protocol_for_England.pdf
(3) WHO Guidelines on Hand Hygiene in Health Care. World Health Organisation. https://s3.xopic.de/openwho-public/courses/4e5GYK9SD83Ju3YhZ4W9eO/rtfiles/27ODaS0EmK51Hyc9soKVv8/9789241597906_eng.pdf
(4) Tackling drug-resistant infections globally: Final report and recommendations. The review on antimicrobial resistance. May 2016 https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf
(5) Modelling the annual NHS costs and outcomes attributable to healthcare- associated infections in England. Guest JF, et al. BMJ Open 2020;10:e033367. doi:10.1136/bmjopen-2019-033367 https://bmjopen.bmj.com/content/10/1/e033367
(6) National Standards of Healthcare Cleanliness 2021. NHS England and NHS Improvement April 2021 https://www.england.nhs.uk/wpcontent/uploads/2021/04/B0271-national-standards-of-healthcare-cleanliness-2021.pdf
Please note: This is a commercial profile