GreenLight Pharmaceuticals Ltd is advancing clinical research and education in UK and Ireland; Though government progress on access and prescribing recommendations lags behind much of Europe
GreenLight and Medical Cannabis
Established in 2014, GreenLight Pharmaceuticals Ltd is an Irish biopharmaceutical company focused on developing safe and effective plant-based medicines. GreenLight specialises in phytocannabinoid research and clinical development.
‘Medical cannabis’ (cannabis-based medical products (CBMP)) refers to a range of products that contain active compounds (primarily Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD)), either synthesized chemically, isolated from plant or raw plant preparations.
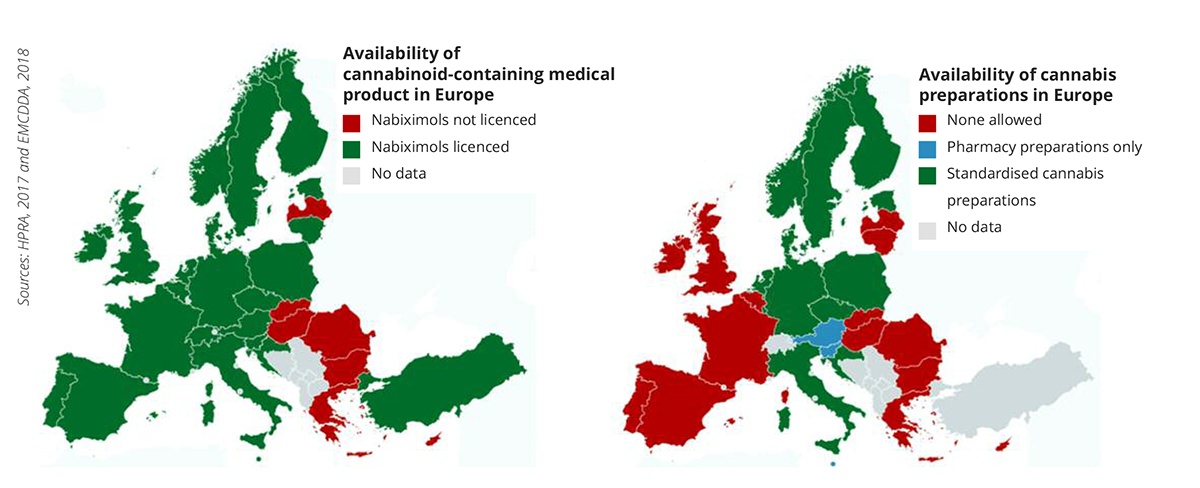
In the past decade Germany, Italy, France, Spain and Switzerland have implemented medical cannabis access programmes for particular indications (Figure 1). In 2018 Ireland and UK also permitted medical use, however, the prescribing process is still nascent, restricting access and uptake.
This article briefly explores the current clinical evidence, issues in the UK and Irish patient access and medical education programmes, with GreenLight’s plans highlighted.
Clinical Evidence for Medical Cannabis
Albeit ‘moderate’ in nature, the strongest evidence of CBMPs clinical efficacy stems from systematic reviews of randomised controlled trials (RCTs). Multiple sclerosis, pain and epilepsy are conditions consistently cited in government reports from Europe and U.S. as the most appropriate to target with medical cannabis.
Multiple Sclerosis (MS)
Standardised cannabis plant extracts of THC and CBD delivered in equal quantities (nabixomols) were the first CBMP to be licensed in the UK for MS-related muscle spasm and neuropathic pain. MS patients receiving nabiximols as an adjunct treatment report reduced spasm versus standard treatment. In 2014 nabiximols were licensed in Ireland, however, the Health Service Executive do not currently deem it to be cost-effective.
Chronic pain
Chronic pain, including neuropathic and musculoskeletal pain is a major reason that patients cite for accessing medical cannabis in Canada and the US. A 2018 Cochrane review reports a modest but significant increase in the proportion of patients who achieve a 30% reduction in pain. GreenLight is optimising clinical trial designs to test cannabinoid combinations for pain in arthritis.
Epilepsy
A 2018 systematic review, of intractable childhood epilepsy RCTs, concludes that adding CBD to conventional anti-epileptic drugs significantly reduces seizure frequency (48.5% of patients reported 50%+ reductions in seizure frequency). GreenLight plan to add to the limited knowledge in this condition by conducting dose-finding trials to minimise interactions with co-medications, in other forms of epilepsy.
GreenLight are already screening the efficacy of lesser-studied cannabinoids from their cultivation programme in 3 core disease areas:
- Neurological conditions – Alzheimer’s, addiction and pain.
- Inflammatory conditions- rheumatoid arthritis, arthritis-related depression, eye disease and diabetes.
- Cancer- of the prostate.
Access Programmes and Medical Education
A range of medical cannabis regulatory frameworks and provision models are currently employed across Europe, with varying degrees of patient accessibility. As UK and Ireland have only recently approved medical cannabis, much progress is needed to operate as effectively as established European programmes (Figure 1). GreenLight Pharma is actively engaging regulators to improve patient access programmes. The current frameworks are briefly contrasted with Germany below.
United Kingdom
In November 2018 medical cannabis was moved from schedule 1 (no medicinal value) to schedule 2, allowing specialist doctors to prescribe for any condition, and for clinical research to be conducted. Since the reschedule, 18 private (no NHS) prescriptions for standardised plant preparations have been made. Doctors are wary to prescribe for a multitude of reasons including the modest evidence base, lack of NHS reimbursement and no NICE prescribing guidance (due Oct. 2019). Importantly, GreenLight’s clinical trials will evaluate safety alongside clinical efficacy and cost-effectiveness of CBMPs.
Ireland
In 2017 a HPRA report recommended that medical cannabis should be prescribed in a limited number of medical conditions, where prior treatment has failed. Specified conditions include MS spasticity, intractable cancer nausea and refractory epilepsy. The Access Programme for medical cannabis is embryonic and currently limited in uptake. Prescribing doctors need to secure a licence for named patients from the Minister for Health. Irish supplies of medical cannabis have only recently been secured, with a small number of patients permitted to use cannabis products from the Netherlands. Announcement of a formal access programme is expected in mid-2019.
Germany
Germany has followed a similar legal framework to the Netherlands with the 2017 Cannabis as Medicine act. Patients with treatment-refractory conditions can access nabiximols, dried cannabis plant or standardised extracts prepared in pharmacies. Prescription is not limited to specialist doctors, nor for specific indications. Germany has tendered for domestic production of up to 2 metric tons of cannabis per anum to standardise the quality of supplies. GreenLight are developing cultivation licences in several countries in Europe and have secured supplier agreements to ensure sustainable, high-quality supplies.
Prescribing guidance needed
Training on CBMPs in the UK is yet to be commissioned by the NHS. In Ireland, the HPRA Medical Cannabis access programme has published detailed guidelines on CBMPs prescribing. Several medical professional organisations have developed clinical advice on CBMPs. Complementing these efforts, GreenLight has compiled an online course on cannabinoid prescribing, which will be launched in autumn 2019.
It is clear that frameworks for medical cannabis access remain underdeveloped in the UK and Ireland. However, GreenLight is actively leading improvements in medical training, prescription recommendations, standardised supplies and robust clinical trials to help develop access systems that fit regulatory requirements, while meeting patient and clinician demand for safe and effective medicines.
Please note: This is a commercial profile
David Gibson, PhD
Chief Scientific Officer
GreenLight Medicines (trading name of GreenLight Pharmaceuticals Ltd)











Meanwhile, tens-of-thousands of desperate patients are still either growing their medicine themselves or buying it from the black market. GPs could prescribe Bedrocan if they had the will and determination to do so but they are essentially being denied that by an establishment still in the grip of Reefer Madness. Supposedly only British evidence of the efficacy and safety of cannabis medicine can determine whether it be prescribed more widely whilst it is being made available to private patients aka those who can afford it. Just another national disgrace.
I’m 1 of many people still waiting for the uk government and doctors to do the right thing and let us with real illnesses to have the medication we really need.
What’s the harm?
I suffer from epilepsy, bad spinal arthritis to a point I can’t sleep for more than 2/3hours per night if that.
My legs are getting worse with the numbness and spasms that I can’t trust myself doing anything without some sort of cannabis!
It’s not nice when you’re a full grown family man and can’t do a thing with your kids.
I was on the “so called” medical cannabis list but got removed because nobody can prescribe it, Why? My life’s a nightmare and I can’t risk putting my kids in danger over something that should be legal!!
The uk needs to join the rest of the world instead of living years behind because it’s seen as something very bad. I’d rather have cannabis than drink alcohol or smoke cigarettes