Leading pancreatic cancer experts Professor Matthias Löhr and Professor Monique van Leerdam of United European Gastroenterology’s (UEG) Public Affairs Committee discuss the importance of early diagnosis and the latest developments in treatment for pancreatic cancer
Pancreatic cancer has the lowest rate of survival amongst all cancers across Europe.1 In the EU alone, it is responsible for over 95,000 deaths every year2 and life expectancy at the time of diagnosis is less than 5 months.3 Recent estimates have indicated that the number of pan-European deaths caused by pancreatic cancer overtook breast cancer fatalities in 2017, placing the condition as the third leading cause of cancer-related deaths.2 There have been few advancements in patient outcomes over the last four decades with mortality rates having seen no improvement and just 3% of patients diagnosed with pancreatic cancer surviving beyond five years.4
How can we turn the tide against Europe’s deadliest cancer?
Professor Matthias Löhr
“One of the biggest challenges concerning pancreatic cancer is awareness. Understanding of the condition, including its symptoms which are notoriously difficult to identify, is alarmingly low. This, combined with the severity means most patients have little or no hope of long-term survival at the point of diagnosis.
Perhaps the most significant consequence of poor awareness around pancreatic cancer is that it prevents early detection of the disease, particularly amongst those at highest risk. Early diagnosis is crucial to delivering improved patient outcomes in all cancers, but particularly so in pancreatic cancer given the cripplingly low survival rates.
It is estimated that two-thirds of the major risk factors associated with pancreatic cancer could be modifiable, providing an opportunity for preventing the disease.5 However, to convert this into reality rather than potential, we need to drive awareness so that people know what to look out for.
The risk factors associated with pancreatic cancer include smoking, chronic pancreatitis, diabetes, obesity and a family history of the condition, whilst incidence rates increase with age. Smoking is related to 20% of all pancreatic cancer cases and causes a 75% increase in the risk when compared with non-smokers.6 Obese patients are found to have a 47% higher risk as opposed to patients with a healthy BMI.7 Having a parent, sibling or child with pancreatic cancer makes the risk of being diagnosed with the condition 2-3 times higher,8 and it is believed that up to 10% of cases are linked to genetic conditions.9
The symptoms of the disease include jaundice, nausea, a change in bowel habits, abdominal and back pain, and unexplained weight loss. Crucially, these are all non-specific which compounds the issue around a lack of awareness and demonstrates why education needs to improve.
Research has shown that pancreatic cancer can be present in the body for many years before patients fall ill or display symptoms.10 The condition is therefore often asymptomatic, and in those cases where symptoms are detected it is typically at an advanced stage and too late to treat successfully. Problematically, this means that a critical opportunity for early detection is often missed. This complexity explains the main reason for slow progress in improving mortality rates.
Improvements in outcomes for patients have stalled over the past 40 years, which can be starkly contrasted to the survival rates seen with other types of cancer. This is partly down to the difficulties in detecting the disease, but is also down to a lack of targeted initiatives devoted to pancreatic cancer and the fact that only select countries have deployed registries to collect data.
Limited funding for research has also contributed to patient outcomes not improving further. While the number of deaths has almost doubled in the past three decades, European funding for the disease only accounts for 2% of the total for all cancers.1 Forecasts predict that there is no sign of this situation improving with the number of cases and deaths from the condition both estimated to increase by 40% by 2035.11 It is therefore essential that more funding is delivered for research.
While the burden currently posed by pancreatic cancer is severe, it is currently not feasible to implement population-based screening for the disease, placing an emphasis on the need for new treatment options.”
Professor Monique van Leerdam
“New and improved treatments will be key to securing improved outcomes patients moving forward. To help this process, it is important to maximise what is known about the different subgroups of pancreatic cancer patients, particularly which groups are benefitting most from what treatment, as this helps to inform treatment pathways and maximise positive outcomes for patients.
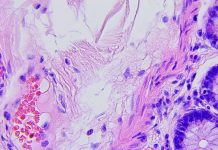
Pancreatic cancer occurs when malignant cells begin to form and multiply in the tissues of the pancreas, which is an organ found behind the stomach. It is increasingly being recognised as a systemic disease made up of micro-metastases when diagnosed. Consequently, a combination of treatments rather than just resection – known as multimodality therapy – is now seen as the first-choice treatment. Within this, neoadjuvant therapy, which serves to shrink tumours as a first step prior to surgery, is now preferred as it can be used to treat the disease earlier. By reducing the size of the tumour, clearer resection can be achieved helping to improve patient outcomes. However, this therapy is still in urgent need of more funding to help improve the precision of staging tools, confirm the correct treatment schedule and reduce toxicity. Only then can the impact of neoadjuvant therapy be maximised.
It is also important that we enable the centralisation of care patients moving forward. In Finland for instance, a law is in place that ensures that patients only receive treatment at five specialised hospitals as part of a strategy to centralise care.1 This is a promising step in the right direction but needs to be replicated across Europe if we are to achieve optimal patient care.
Where research has been commissioned for pancreatic cancer it has yielded important developments. One study has shown that removing bacteria from the gut and pancreas has slowed cancer growth and reprogrammed immune cells to react against cancer cells.12 These findings are significant and could be practice-changing as the removal of certain bacterial species could enhance the efficacy of chemotherapy or immunotherapy. This means there is the potential for increasing patients’ good bacteria in order to slow tumour growth or decrease pancreatic cancer risk. Another study revealed that serum MIC-1 levels may present a new diagnostic biomarker for the early detection of pancreatic cancer.13 Lastly, research into imaging has shown that diagnosis could also be improved using positron emission tomography techniques where computed tomography and endoscopic ultrasound are not completely diagnostic.14
The development of imaging has become increasingly important, not just for the diagnosis, but also for achieving the best treatment and management decisions. While multidetector computed tomography (MDCT) is the current imaging tool of choice for pancreatic cancer assessment, ultrasonography, endoscopic ultrasound, contrast-enhanced ultrasound, and MRI with MRCP can help compliment this with more detailed information. This multimodality approach has seen considerable improvements in recent times, but each imaging tool has its own purpose, advantages and disadvantages across the diagnosis, treatment and management of pancreatic cancer. Again, it is paramount that more dedicated funding is provided so that clinicians are given the means to effectively evaluate the available pancreatic imaging modalities and apply the relevant options as required.
Ultimately if we are to comprehensively address the pancreatic cancer burden facing Europe, we need to drive more funding, defined strategies and treatment innovation for the condition. The lack of improvement in patient outcomes over the last four decades cannot be ignored and we must act now.”
References:
- (2018). Pancreatic Cancer Across Europe. Available: https://ueg.eu/files/771/b7ee6f5f9aa5cd17ca1aea43ce848496.pdf
- European Commission . (2018). European Cancer Information System. Available: https:// ecis.jrc.ec.europa.eu/explorer.php?$0-0$1-AE28$2-All$4-1,2$3-All$6-0,14$5-2008,2008$7-8$CEstByCancer$X0_8-3$CEstRelativeCanc$X1_8-3$X1_9-AE28.
- Ferlay J., Partensky C., Bray F. More deaths from pancreatic cancer than breast cancer in the EU by 2017. ACTA Oncologica, August 2016.
- Roser, M., Ritchie, H., . (2015). Cancer. Available: https://ourworldindata.org/cancer.
- Iodice, S., Gandini, S., Maisonneuve, P., Lowenfels A, B. (2008). Tobacco and the risk of pancreatic cancer: a review and meta-analysis.. Send to Langenbecks Arch Surg. 393 (4), 535-545.
- Bosetti, et al. (2012). Cigarette smoking and pancreatic cancer: an analysis from the International Pancreatic Cancer Case-Control Consortium. Annals of Oncology. 23 (7), 1880-1888
- Pancreatic Cancer Action Network . (2018). 16 Pancreatic Cancer Warning Signs Infographic. Available: https://www.pancan.org/spread-the-word/16-pancreatic-cancer-warning-signs-infographic/
- Pancreatic Cancer UK . (2018). Family history of pancreatic cancer. Available: https://www.pancreaticcancer.org.uk/information-and-support/facts-about-pancreatic-cancer/family-history-of-pancreatic-cancer/
- Salvatore, T., . (2015). Pancreatic cancer and diabetes: A two-way relationship in the perspective of diabetologist. International Journal of Surgery. 21 (1), 72-77.
- Canto, M, I. et al . (2014). International Cancer of the Pancreas Screening (CAPS) Consortium summit on the management of patients with increased risk for familial pancreatic cancer . GUT. 62 (3), 339-347
- World Health Organization. (2018). CANCER TOMORROW. Available: http://globocan.iarc.fr/Pages/burden_sel.aspx
- Pushalkar, S. et al . (2018). The Pancreatic Cancer Microbiome Promotes Oncogenesis by Induction of Innate and Adaptive Immune Suppression. Cancer Discov.. 403 (4), 403-416.
- Koopmann J, Rosenzweig CN, Zhang Z, et al. Serum markers in patients with resectable pancreatic adenocarcinoma: macrophage inhibitory cytokine 1 versus CA19-9. Clin Cancer Res2006;12:442-6.
- Lee, E.S. and Lee, J.M. (2014). Imaging diagnosis of pancreatic cancer: A state-of-the-art review. World J Gastroenterol. 20(24), 7864–7877.