Hernando Lopez-Bertoni, explores the new wave of molecular cancer therapeutics and states the case for learning the mechanisms as a pro, so one can target them as an artist
Hernando Lopez-Bertoni 1,2
1 Hugo W. Moser Research Institute at Kennedy Krieger, 707 N. Broadway, Baltimore, MD, U.S. 21205; Department of 2 Neurology, Johns Hopkins School of Medicine, 600 N. Wolfe Street, Baltimore, MD, U.S. 21287.
Cancer stem-cell (CSC) phenotype, cellular heterogeneity & GBM
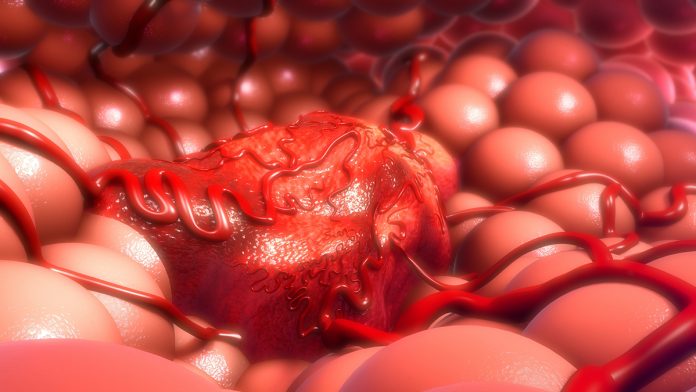
Intra-tumour heterogeneity presents one of the biggest challenges in the development of solid cancer therapeutics. Cells within the same tumour display distinct phenotypes that affect their growth rate, survival, migration, therapy-response and tumour-propagating capacity 1. We now understand cells within the tumour endowed with stem cell properties (i.e. cancer stem cells or CSCs) play critical roles in driving intra-tumour cellular heterogeneity by establishing dynamic cellular transitions within tumours.
These cells display the ability to switch cellular phenotypes and can transition between stem-like and non-stem-like states depending on cell-intrinsic and extrinsic factors, including current therapeutics designed to get rid of the tumour itself 2. The acquisition of a stem-like phenotype is a key event determining therapy-resistance in cancer cells 3. This ability to switch between cellular states make cancer cells a moving target that can diminish the impact of current therapeutics.
GBM are highly aggressive tumours that display a poorly differentiated cell phenotype characterised by high expression of genes enriched in embryonic stem cells (ESCs) 4. Lineage-tracing experiments show that stem-like cells are responsible for GBM re-growth after therapy and this process is in part mediated by known drivers of stemness (e.g. Sox2) 5. Transcriptome analysis of clinical samples identified distinct GBM subtypes based on molecular signatures (i.e. mesenchymal, classical, and proneural) 6 with the mesenchymal subtype, thought to be the most aggressive, sharing a high degree of similarity with stem cells at the transcriptome and epigenetic level 7.
Single-cell transcriptome analysis shows GBM cells exist in at least four different cellular states and can transition dynamically between molecular subtypes depending on cell-intrinsic and extrinsic factors 8. This high degree of transcriptional and chromatin adaptability is thought to influence the emergence of therapy-resistant GBM cell sub-populations 3.
It is, therefore, imperative that we understand the molecular mechanisms underlying glioma-stem cell (GSC) plasticity to design rational therapeutics aimed at stopping the conversion of non-GSCs to GSCs to limit intra-tumour heterogeneity, eliminate transitions between cellular states and block the emergence of therapy-resistant cells.
Attacking the moving target
Over the last two decades, our molecular understanding of RNA interference (RNAi) and the technology to deliver oligonucleotides in vivo has grown exponentially 9. The growing appeal of using RNAi technology as therapeutics is based, in large part, on the potential to achieve highly specific, rationally designed therapies based on the primary sequence of the targeted transcripts. The use of this technology allows for the possibility to target disease-specific undruggable molecular events providing new options for treatment. One RNAi modality that is gaining pre-clinical traction as a promising new treatment approach for cancer are microRNAs (miRNAs).
We recently identified a mechanism that drives the stem cell phenotype of GBM cells that can repress miRNAs (i.e. miR-148a and miR-296-5p) that modify the DNA methylation landscape, chromatin structure and induce the tumour propagating capacity of GBM cells. Importantly, reconstituting these miRNAs in pre-established GBM xeno-grafts inhibits tumour propagating capacity in vivo and the prolongation of animal survival 10,11.
These results highlight that identifying epigenetic regulators that control GSC plasticity can provide new avenues to treat tumours, such as GBM.
What is the next step for miRNA-based therapeutics?
One feature of miRNAs that is frequently overlooked concerns the ability of one miRNA to target multiple mRNA transcripts. This promiscuous quality of miRNAs allows for the selection of one miRNA to target multiple mRNAs dysregulated during tumourigenesis. This approach can allow the targeting of multiple parallel oncogenic pathways using a single agent, enhancing therapeutic efficacy and reducing the chances of tumour recurrence. Single-cell sequencing technology is rapidly expanding and providing unprecedented molecular resolution of disease conditions, including cancer.
These approaches are yielding high-resolution maps of cellular states within tumours and emerging bioinformatic approaches allow us to model heterogeneity as a dynamic network and infer tumour evolution 12.
Integrating single-cell sequencing data, knowledge of the different cellular states in a disease condition and bioinformatics allows for an agnostic approach to selecting miRNAs with therapeutic potential. One can now envision using this high-resolution transcriptome data to select miRNAs that block critical oncogenic pathways at multiple nodes within cell subsets to eliminate cell populations deemed critical for tumour growth, propagation and the emergence of therapy-resistance. This rational “top down” approach to using miRNAs as therapeutic tools has the potential to significantly advance the development of next-generation molecular therapeutics.
We are now well underway in an exciting time for cancer research, especially relating to the development of targeted therapies. As our knowledge of how miRNA targetomes contribute to disease increases and technological advances to deliver miRNAs in vivo advance, we envision an explosion of RNAi-mediated pre-clinical therapeutics for cancer that combines single-cell sequencing data, bioinformatics, and advanced nanocarriers for in vivo delivery.
Acknowledgement
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute of Health (NIH) [1 R01 NS120949-01 (Lopez-Bertoni)].
References
1 Navin, N. et al. Tumour evolution inferred by single-cell sequencing. Nature 472, 90-94, doi:10.1038/nature09807 (2011).
2 Auffinger, B. et al. Conversion of differentiated cancer cells into cancer stem-like cells in a glioblastoma model after primary chemotherapy. Cell Death Differ 21, 1119-1131, doi:10.1038/cdd.2014.31 (2014).
3 Liau, B. B. et al. Adaptive Chromatin Remodeling Drives Glioblastoma Stem Cell Plasticity and Drug Tolerance. Cell Stem Cell 20, 233-246 e237, doi:10.1016/j.stem.2016.11.003 (2017).
4 Brown, D. V. et al. Expression of CD133 and CD44 in glioblastoma stem cells correlates with cell proliferation, phenotype stability and intra-tumor heterogeneity. PLoS One 12, e0172791, doi:10.1371/journal.pone.0172791 (2017).
5 Gangemi, R. M. et al. SOX2 silencing in glioblastoma tumor-initiating cells causes stop of proliferation and loss of tumorigenicity. Stem Cells 27, 40-48, doi:10.1634/stemcells. 2008-0493 (2009).
6 Verhaak, R. G. et al. Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell 17, 98-110, doi:10.1016/j.ccr.2009.12.020 (2010).
7 Malta, T. M. et al. Machine Learning Identifies Stemness Features Associated with Oncogenic Dedifferentiation. Cell 173, 338-354 e315, doi:10.1016/j.cell.2018.03.034 (2018).
8 Neftel, C. et al. An Integrative Model of Cellular States, Plasticity, and Genetics for Glioblastoma. Cell 178, 835-849 e821, doi:10.1016/j.cell.2019.06.024 (2019).
9 Alzhrani, R. et al. Improving the therapeutic efficiency of noncoding RNAs in cancers using targeted drug delivery systems. Drug Discov Today 25, 718-730, doi:10.1016/ j.drudis.2019.11.006 (2020).
10 Lopez-Bertoni, H. et al. Sox2 induces glioblastoma cell stemness and tumor propagation by repressing TET2 and deregulating 5hmC and 5mC DNA modifications. Signal Transduct Target Ther 7, 37, doi:10.1038/s41392-021-00857-0 (2022).
11 Lopez-Bertoni, H. et al. Bioreducible Polymeric Nanoparticles Containing Multiplexed Cancer Stem Cell Regulating miRNAs Inhibit Glioblastoma Growth and Prolong Survival. Nano Lett 18, 4086-4094, doi:10.1021/acs.nanolett.8b00390 (2018).
12 Larsson, I. et al. Modeling glioblastoma heterogeneity as a dynamic network of cell states. Mol Syst Biol 17, e10105, doi:10.15252/msb.202010105 (2021).
*Please note: This is a commercial profile
© 2019. This work is licensed under CC-BY-NC-ND.