Thomas Münzel MD, Andreas Daiber PhD, Ulrich Pöschl PhD and Jos Lelieveld PhD discuss the link between air pollution and cardiovascular disease in Europe
By way of an introduction, ambient and household air (indoor air) pollution are considered to be major health risk factors leading to morbidity and premature mortality with significant direct and indirect costs to the community1. The World Health Organization (WHO)2 and the Global Burden of Disease (GBD) project1 calculated for 2015, 4.2 million premature deaths per year worldwide due to air pollution especially by particulate matter with an aerodynamic diameter < 2.5 µm (PM2.5). More than half of the deaths were the result of cardiovascular diseases such as coronary heart disease and cerebrovascular disease due to embolic and hemorrhagic stroke but also due to other non-communicable diseases such as arterial hypertension, diabetes, lung cancer and chronic obstructive pulmonary disease.
Death rates due to air pollution are significantly higher than previously thought
In 2018 and 2019, two new studies calculated a much higher mortality and morbidity burden than previously thought, in particular due to the use of a new and much more accurate hazard ratio function of the PM2.5 concentration-response association, the GEMM. 3, 4 This model has a number of advantages over the Integrated Exposure-Response Function (IER) formerly used by the WHO and GBD and is now considered by both WHO and GBD to calculate premature mortality. Richard Burnett’s GEMM is based on the analysis of much larger and geographically extended epidemiological data obtained from 41 cohort studies from 16 countries.3 This implies the inclusion of an additional 20 000 cases and 2.5 million deaths from study data from heavily polluted and densely populated countries such as China, whereas the WHO-GBD-IER mainly covered data from less polluted western regions such as Europe, Canada and the U.S.
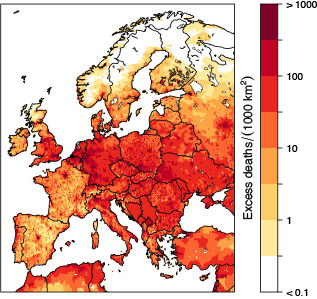
Image: © 2019, Oxford University Press
In addition, IER mortality has been reported to be based on five major causes including coronary heart disease, cerebrovascular disease, chronic obstructive pulmonary disease, lung cancer and lower respiratory tract disorders, while in the study by Burnett et al.3 the development and application of GEMM was based on worldwide mortality data from all non-communicable diseases as well as pneumonia. The estimated additional air pollution death rate was 8.9 million, more than twice that of the GBD and WHO (4.2 million).
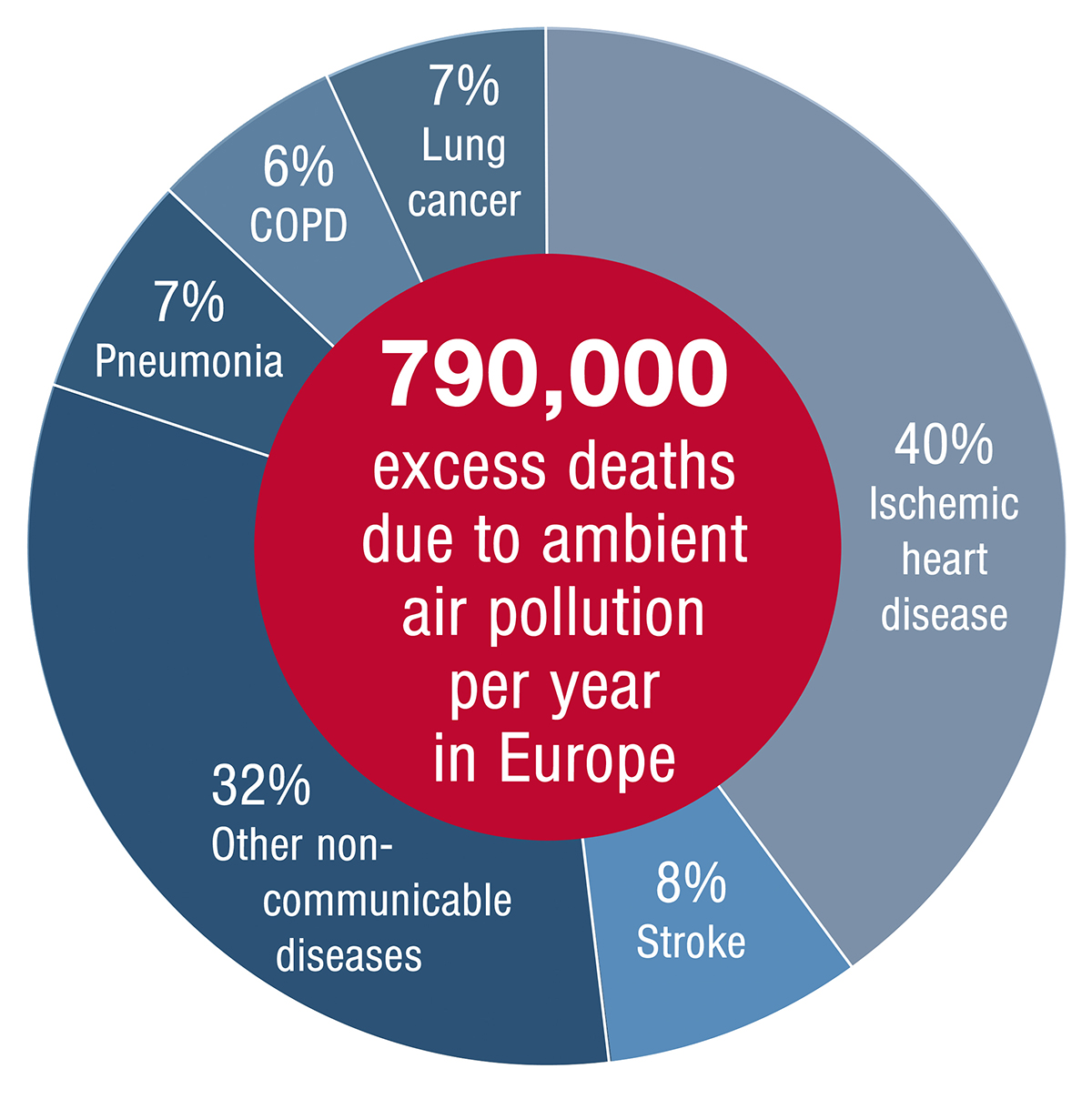
Image: © 2019, Oxford University Press
Recently, Lelieveld et al.4 calculated that, based on the GEMM for Europe, this would result in up to 790,000 premature deaths per year mostly due to PM2.5 exposure, more than twice based on the previous GBD-IER estimate (269,000) (Figures 1 and 2). Interestingly, the highest numbers of premature deaths occurred in Germany (154 per 100,000 per year), followed by Poland (150), Italy (136), France (105) and the United Kingdom (98)4 (Table 1). The main part of the mortality was due to cardiovascular diseases. As estimated by Jos Lelieveld et al. , PM2.5 air pollution reduces the European average life expectancy by 2.2 years.4 To put this into perspective, the WHO estimates that the excess death rate from tobacco smoking is 7.2 million per year; hence, air pollution globally is now rated as the larger risk factor.
Effects of air pollution on the cardiovascular system
When discussing the pathophysiological effects of air pollution, we focus on PM2.5 because, in particular, the small particulate matter particles can penetrate deeply into the lungs. Following inhalation of PM2.5, the fine aerosol particles are released into the bloodstream via a transition process and then absorbed into the blood vessel.5-7 The particulate matter in the vessel wall stimulates the formation of reactive oxygen species, i.e., pro-oxidative substances and pro-inflammatory biological mediators (i.e., such cytokines as interleukin-6 and tumor necrosis factor) and acute phase proteins such as the C-reactive protein and the vasoconstrictor hormone endothelin.5-7 These processes initiate or accelerate atherosclerotic changes. In general, the smaller the particle is (down to ultrafine particles <0.1µm, PM0.1), the higher the probability of a rapid translocation of the particles into the vessel wall.7
Furthermore, activation of blood coagulation is observed. Accordingly, high levels of PM2.5 are accompanied by hypercoagulation biomarkers, such as high plasma levels of fibrinogen and D-dimer and increased thrombin formation.5-7 Human data show an inverse relationship between PM exposure and heart rate variability.5-7 PM2.5 can induce arterial hypertension via direct sympathetic activating effects in the brain6,7 or by triggering endothelial dysfunction due to decreased vascular nitric oxide (NO) bioavailability.7
The particulate matter limits for Europe are too high
In view of the WHO recommended guideline of 10 μg m3 for PM2.5, it can be assumed that more than 91% are exposed to higher concentrations worldwide. The European Union (EU) has been applying a mean air quality limit of 25 μg/m3 for PM2.5 since 2015, which is 2.5 times higher than the WHO guideline of 10 μg/m3. The target is 20μg/m3 by 2020, which is considered too high as well due to the new data. For comparison, the annual average limit in the US is 12 μg/m3 (since 2012) and in Canada 10 μg/m3 (since 2015), which are to be further reduced in the future. In Australia, the annual PM2.5 limit is 8 μg/m3, which should be further reduced to 7 μg/m3 by 2025.
Key points:
- Due to air pollution (PM2.5 and ozone), there are 8.9 million deaths per year worldwide.
- Almost 800,000 premature deaths per year are calculated in Europe, with coronary heart disease and stroke predominating, especially with around 50% of premature deaths.
- The number of deaths from particulate matter worldwide exceeds the number of deaths caused by smoking.
- The limit for Europe must, therefore, be drastically reduced
- Air pollution must be recognised as a cardiovascular risk factor and be mentioned in the guidelines of the European Society of Cardiology for Prevention, Heart Attack and Stroke and evaluated accordingly.
References
1 Cohen AJ, Brauer M, Burnett R, et al.: Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 2017; 389: 1907-18.
2 https://www.who.int/gho/phe/outdoor_air_pollution/burden/en/ . 2016.
3 Burnett R, Chen H, Szyszkowicz M, et al.: Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc Natl Acad Sci U S A 2018; 115: 9592-7.
4 Lelieveld J, Klingmuller K, Pozzer A, et al.: Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. European heart journal 2019.
5 Munzel T, Sorensen M, Gori T, et al.: Environmental stressors and cardio-metabolic disease: part I-epidemiologic evidence supporting a role for noise and air pollution and effects of mitigation strategies. European heart journal 2017; 38: 550-
6 Munzel T, Sorensen M, Gori T, et al.: Environmental stressors and cardio-metabolic disease: part II-mechanistic insights. European heart journal 2017; 38: 557-64.
7 Munzel T, Gori T, Al-Kindi S, et al.: Effects of gaseous and solid constituents of air pollution on endothelial function. European heart journal 2018; 39: 3543-50.
Professor Thomas Münzel
University Medical Center of the Johannes Gutenberg-University Mainz
Department of Cardiology
Tel: +49 613 117 7250
Professor Jos Lelieveld
Max Planck Institute for Chemistry,
Johannes Gutenberg University Mainz
Please note: This is a commercial profile








