New research finds that bleeding and stroke are COVID-19 brain complications that are more frequent in people with diabetes and hypertension
While COVID-19 continues to ravage the majority of the world and vaccines are taking their first bows on the clinical trial stage, the undercurrents of this new virus are moving swiftly throughout the medical community.
Cancer deaths increased in the UK, due largely to a fear of catching COVID-19 when coming in for consultations or treatment. People continue to be fearful for their personal health situations. The list of those who are vulnerable to COVID-19 is largely known, but there are anomalies that create further questions about how the virus attacks the human body.
Right now, researchers have published well above 6000 journal articles on the various ways that COVID-19 can cause complications for health and social care – but, as the days go on, more undercurrents are waiting to reveal themselves. COVID-19 patients with diabetes and heart problems have been marked out as highly vulnerable to a more severe form of COVID-19, resulting in hospitalisation and even death.
Writing for us in September, Dr Lucy Chambers, Head of Research Communications at Diabetes UK, said: “Large UK population studies have consistently shown that people with diabetes are at increased risk of dying from the virus. Research by the NHS found that those with type 1 have 3.5 times the risk and those with type 2 twice of dying compared to people without the condition.
“We know that age is the dominant risk factor, with the vast majority of deaths occurring in the 70 years plus age groups. We’ve also learnt that ethnicity, socioeconomic status, sex, bodyweight, long-term blood sugar control and a whole host of other factors contribute to the huge variation in individual risk between people with diabetes.”
The new research into COVID-19 brain complications
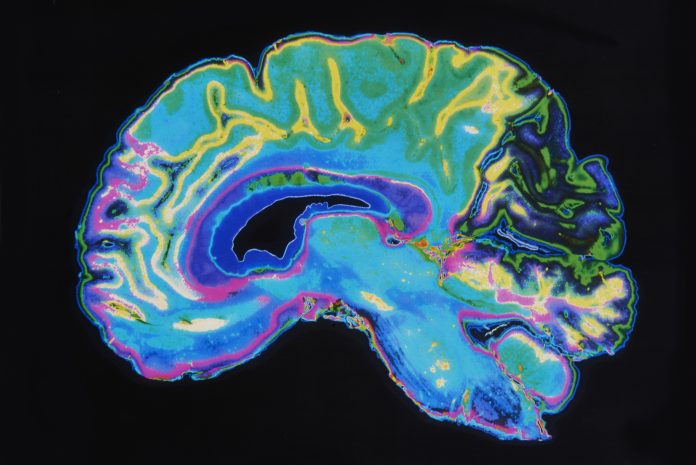
Dr Freeman and colleagues in the Perelman School of Medicine at the University of Pennsylvania looked at COVID-19 patients who underwent head CT or MRI in their health system from January to April 2020. Of the 1,357 patients with COVID-19 admitted to the system in those four months, 81 had a brain scan performed. The most common reasons for the brain scans were altered mental state and focal neurological deficits such as speech and vision problems.
“COVID-19’s effects extend far beyond the chest,” said study lead author Colbey W. Freeman, MD, chief resident in the Department of Radiology at Penn Medicine in Philadelphia.
“While complications in the brain are rare, they are an increasingly reported and potentially devastating consequence of COVID-19 infection.”
Two thirds of patients with critical brain results were African American
Out of 81 patients with brain scans, 18, or just over one in five, had findings that were considered emergency or critical, including strokes, brain bleeds and blocked blood vessels. At least half the patients had pre-existing histories of high blood pressure and/or type 2 diabetes. Sadly, three patients with critical findings died while they were participating in the study.
Two-thirds of the patients with critical results in the study were African American, suggesting that these patients also may require closer monitoring – again, ethnicity data is going to be a key protection measure for minorities after this virus is dealt with.
Why is this happening to the human brain?
“When your body is in an inflammatory state, it produces all these molecules called cytokines to help recruit the immune system to perform its function,” Dr Freeman said.
“Unfortunately, if cytokines are overproduced, the immune response actually starts doing damage.”
The exact mechanisms for COVID-19’s harmful neurological effects are not known and may involve multiple factors. However, a popular theory suggests that inflammation associated with the infection itself is why the brain takes such damage. Supporting that idea, the research done by Dr Freeman et al found blood markers of inflammation to be high in people with the worst impacted brains.