Eric Buckland of Translational Imaging Innovations and Ronald Schuchard, Clinical Product Development Expert, explore the benefits of ophthalmic precision medicine to improve patient care across sectors
The term “precision medicine” has become very popular over recent years, driven by scientific and socio-political perspectives. The goal of precision medicine is to improve individual care through the stratification of patients according to a taxonomy derived from large-scale data, including clinical, lifestyle, genetic and further biomarker information, thus going beyond the classical “signs-and-symptoms” approach. Precision medicine is a process that incorporates a comprehensive approach to understanding the specific needs of patients with shared attributes, targeting more effective care with lower risks. Today’s medical records systems are not up to the task. The evolution of precision medicine requires a revolution in managing healthcare data, from clinical research, through clinical trials and into clinical practice.
Innovations in GTx and AI inherently target the holy grail of precision medicine
As promising as Gene Therapy (GTx) and Artificial Intelligence (AI) are to the future of healthcare, the field of ophthalmology has seen one FDA-cleared gene therapy[1] and two FDA-cleared AI diagnostic products[2],[3]. While there are many reasons for the limited progress of precision medicine in ophthalmology, the lack of quality data sources and reproducible processes for leveraging large-scale image-rich data is a major contributing factor.
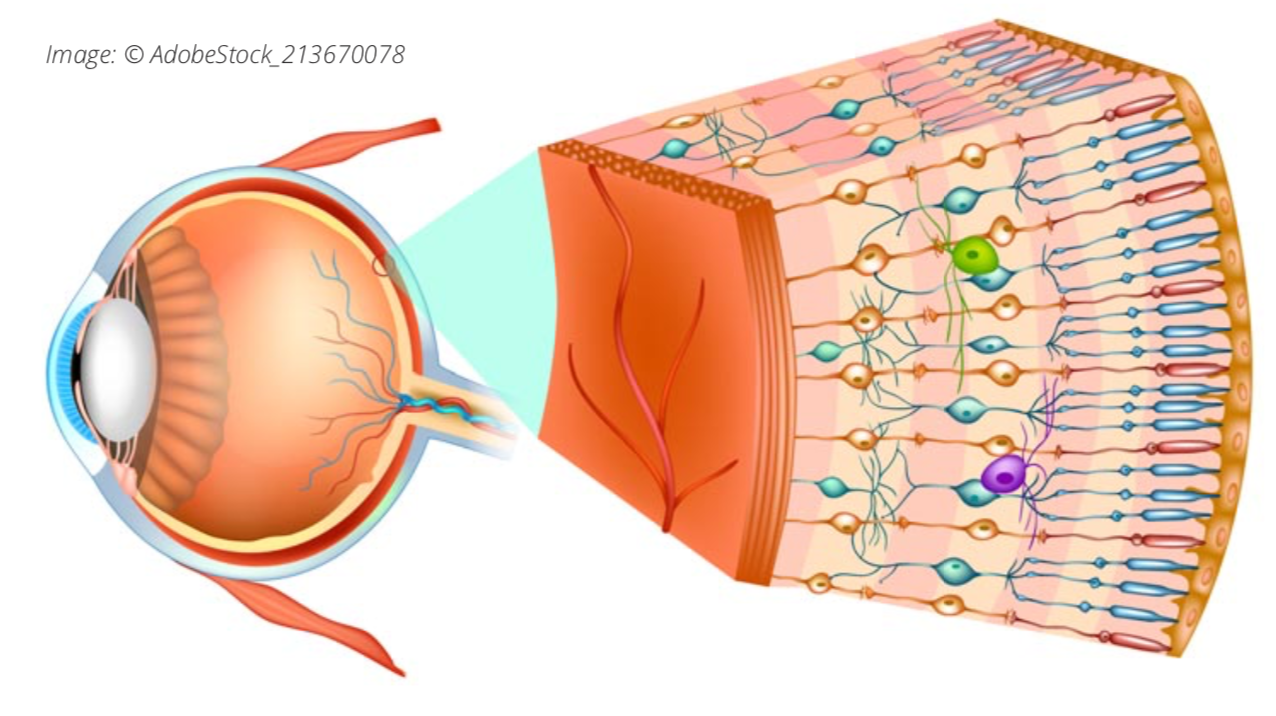
Degenerative ocular diseases, including glaucoma and dry age-related macular degeneration progress “gradually, then suddenly” [4]. This slow progression of disease presents a host of problems in both diagnosis and treatment. Even in cases with clear risk factors and suggestive clinical indications, the lack of treatments mandates a wait-and-see clinical approach. Predictive biomarkers are needed that accurately predict when a patient’s condition will progress to severe vision loss.
The absence of prognostic markers impacts the development of new drugs that might slow, halt, or reverse degeneration
How does one validate a drug that may slow disease progression over decades? How does one assess the risk-benefit trade-offs? In our aging society, progressive vision loss will threaten the quality of life and increase the economic burden on the global economy. This is a real threat that requires new protocols for evaluating drugs and prognostic biomarkers to identify at-risk patients as candidates for a given therapy. Current clinical health records, proprietary imaging devices, and image management systems designed around patient case management are not suited to discovering, validating, and deploying prognostic biomarkers or validating the new class of clinical endpoints required to get ahead of the problem of degenerative eye disease.
Drug molecules and biologics are necessary for a new drug, and clinical endpoints are the outcome measures for assessing safety and effectiveness. Clinical endpoints form a battery of tests that measure structure, function, and impact on activities of daily living at each phase of clinical trials. The US Food and Drug Administration (FDA) provides guidance on selecting endpoints for clinical trials[5]. The primary concern of the FDA is constraining Type I errors – minimizing the risk that an ineffective drug is cleared through the process. The bar is high. The FDA mandates that the probability of clearing an ineffective drug be below one chance in 40. Statistical rigor requires the prospective selection of endpoints and prospective analysis protocols that eliminate statistical inflation and data dredging. Tight control of Type I failures can increase the probability that good treatment candidates end up being rejected – the Type II failures. Developing robust clinical endpoints for slowly degenerative diseases and rare diseases that are candidates for gene therapy is a significant challenge and a major barrier to progress in ophthalmology.
Clinical endpoints are not born; they are made
It is critical to develop appropriate clinical endpoints in parallel with new drug development from the earliest phases. The FDA recognizes primary, secondary, and exploratory endpoints (or endpoint families). The primary endpoint is the main test that a treatment has worked. Secondary endpoints provide evidence of additional clinical benefits or elucidate mechanisms of action; secondary endpoints are only considered following success against the primary endpoint. On the other hand, explanatory endpoints are experimental and provide flexibility to test additional clinical hypotheses and evaluate new biomarkers that may evolve into future primary or secondary endpoints.
New imaging and testing modalities are increasingly moving from the laboratory to clinical trials. Innovative new techniques testing patient sensitivity to light[6] and micromotions of the retina[7] show promise as early markers of disease operating at the eye-brain connection. Such new endpoints do not need to be derived from clinical standards of care. Inclusion as exploratory endpoints in clinical trials maximizes the leverage of expensive clinical trial processes to clear new treatments that benefit patients while advancing the development of future primary and secondary endpoints for degenerative eye disease.
Improving patient care across all sectors
Integrated image and data management across the entire lifecycle of pre-clinical and clinical research, clinical trials, and clinical practice are necessary to advance ophthalmic precision medicine. The more finely grained we stratify patients and target therapies, the more likely we are to realize the value in emerging therapies, improve patient care across all sectors of the population, and ultimately reduce healthcare costs. Finely grained medical solutions require large-data solutions with enough power to discover the needed biomarkers and validate clinical endpoints.
Translational Imaging Innovations is leading the way with comprehensive systems that simplify the capture, curation, and analysis of images and data, with transparency and traceability. Our architecture begins with the TII Data Genome, a scalable and extensible relational data structure supported by the ocuVaultTM database and application programming interface (API). ocuVaultTM simplifies data flows, automates data security, and simplifies database deployment across sites and programs. ocuLinkTM is the TII vendor-neutral, multimodal, data curation, visualization, and annotation application, optimized for large-scale image analysis workflows. Mosaic is the TII computational platform designed for batch processing the multi-stage computational recipes required for biomarker discovery and trial data analysis. At TII, our goal is to enable translational researchers to develop better diagnostics and better therapies, with more predictable benefits – faster, at a lower cost, and with less frustration.
- LUXTURNA, Spark Therapeutics, Inc. https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/luxturna
- IDx-DR, Digital Diagnostics Inc, DEN180001, https://fda.report/DeNovo/DEN180001
- EyeArt, Eyenuk, Inc, K200667, https://fda.report/PMN/K200667
- Ernest Hemingway, The Sun Also Rises
- Draft Guidance for Multiple Endpoints in Clinical Trials, FDA- 2016-D-4460-0002, https://www.fda.gov/media/102657/download
- Aguilar MC, et al, Automated instrument designed to determine visual photosensitivity thresholds. Biomed Opt Express. 2018 Oct 18;9(11):5583-5596.
- Sheehy CK, et al, Fixational microsaccades: A quantitative and objective measure of disability in multiple sclerosis. Mult Scler. 2020 Mar;26(3):343-353.

This work is licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International.