Simon Holt, Honorary Professor at Swansea University, reflects on the key challenges within cancer care and the benefits of genomic testing in improving patient outcomes
UK cancer care needs improving. As of 2019, the UK ranked 33rd out of 41 developed nations for cancer mortality, while the latest figures show that only 59% of patients in England started their first cancer treatment within two months of an urgent GP referral, falling well short of the 85% target.
Many factors contribute to this, including the overuse of chemotherapy, especially in the case of breast cancer. Not only can this harsh and untargeted treatment have a devastating impact on patients, but the University of East Anglia found that it costs the UK economy £141m in productivity every year, with 320,000 workdays lost annually during treatment.
So, what is the solution? Obviously, there isn’t an immediate fix to these issues. However, genomic tests can play a revolutionary role in improving care outcomes and reducing patient suffering associated with chemotherapy, enhancing clinical confidence and cutting costs for the health service. This is particularly relevant to breast cancer, the most common cancer among women.
Reducing unnecessary suffering
The gruelling side effects of adjuvant chemotherapy (meaning when it is given following ablative surgery to help prevent recurrence) on patients are well-documented. Lethargy and loss of appetite are very common, as well as loss of hair, feeling in the fingertips and weight gain. The risks of dementia, depression and anxiety are also increased, while up to 1% could die from complications of the treatment. All this shows that we simply cannot afford to prescribe chemotherapy to people who don’t need it.
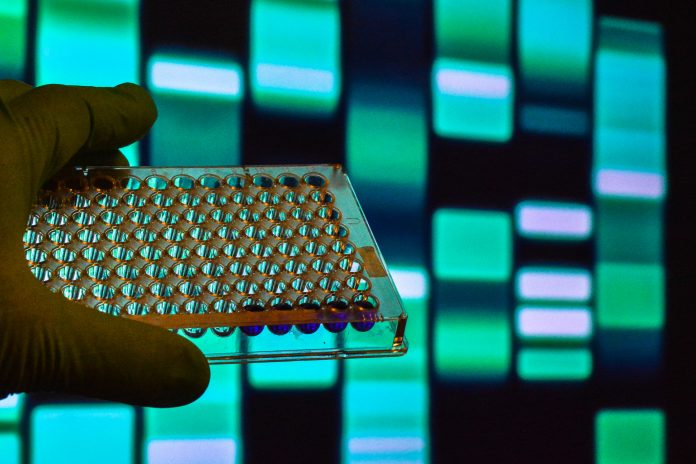
Testing which genes are overactive or have been turned off in breast cancer can provide an accurate guide as to who needs chemotherapy and who does not. Some tests, such as the Oncotype DX test, can identify whether a patient will likely benefit from chemotherapy and help develop personalised treatment plans.
Exact Sciences, the company behind the Oncotype DX test, recently concluded an independent UK multi-centre trial of 680 NHS patients with early breast cancer, where one to three of the under-arm lymph glands were involved. Without the test, 80% of women were advised that they should have chemotherapy, but after taking the test, only 27% were found to need it. This means more than half of the patients were spared chemotherapy treatment by using the test.
The evidence is clear. Genomic testing can reduce unnecessary chemotherapy and improve care outcomes for patients. Promisingly, further research shows that it can positively influence patient and clinicians’ confidence in treatment decisions.
Genomic testing: Improving patient and clinical confidence
A breast cancer diagnosis is devastating. Understandably, patients can feel anxious about their cancer journey and the options available to them, while oncologists often have a complex puzzle to piece together to provide advice on the best course of treatment.
Genomic testing can help to address this anxiety. A UK research study found that 55% of oncologists felt more confident with their chemotherapy recommendation when using the multigene assay. The same research found that patients felt even more reassured, with 71% becoming more confident in their treatment recommendation.
This is despite many being given an initial recommendation that they should receive chemotherapy. The patients clearly valued a more tailored and personalised treatment plan, even when a genomic test showed they could not safely avoid chemotherapy.
Cutting costs
The use of genomic tests can cut costs at a time of increasing financial pressure on the health service. Recent data shows that NHS waiting lists in England have climbed to a new record high of 7.6 million – a figure exacerbated by the pandemic – so solutions that can improve efficiency in any area are desperately needed.
Evidence shows that genomic tests offer significant savings to the NHS – about £770 per patient. Other health economic modelling has found a weighted average saving across node-negative and node-positive patients of £593 per tested individual. This doesn’t include savings on travel expenses, the additional cost of care at home given by family and friends, treating long-term side effects and time off work.
A modelling simulation has also shown that the impact of testing lymph node-positive breast cancer patients from a medium-sized NHS Trust could reduce unnecessary appointments by 41%. This demonstrates the value of genomic testing and the transformative impact that it could have on the NHS.
Treating advanced disease is always far more costly and less effective than prevention or early diagnosis in the non-metastatic phase of a cancer. In patients with breast cancer who are diagnosed early, surgery will often offer a cure. To give additional chemotherapy treatments to those who have already been cured by their surgery is economically wasteful and leads to significant unnecessary suffering for patients.
With genomic testing, many patients can avoid chemotherapy, and oncologists can redirect time to other cancer patients and treatments. The consequence is that the NHS benefits by enabling resources to be concentrated towards those who really need it.
To the future
The prevailing paradigm – giving breast cancer patients chemotherapy to prevent recurrence by default – needs rethinking. We can’t afford to keep overprescribing chemotherapy to people who may not need it. This is not just a matter of cost but also a question of quality of life.
The UK Government and health services must recognise the potential of genomic tests to help transform cancer care to the benefit of patients, oncologists and the broader healthcare system.
In the longer term, I believe developments in genomics and gene expression analysis will lead to the ability to reprogram the patient’s own immune system to recognise and destroy cancers, making chemotherapy rarely necessary.