Dr Gerry Morrow shares his thoughts on the precision medicine, defined as the cost-effectiveness of breakthrough treatments and explains why this area is a priority for both researchers and government
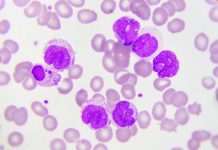
The emergence of precision medicine is upon us. Defined as an approach to patients with specific and identifiable characteristics, which enable a targeted diagnostic or treatment methodology. It has become a priority focus for both researchers and the government.
Within this broader category of precision medicine, there are two defined subcategories, which are precision targeting and breakthrough precision medicine. The distinction between these two categories is critical to their cost-effectiveness and the likely usage of such tests or therapies. (1)
Precision targeting
Precision targeting or stratified medicine describes a process of narrowing the use of conventional medicines and diagnostics based on using information such as pharmacogenomics, medical records and demography.
This process is predicated on three elements. Which are:
- Effective genetic tests to diagnose illnesses reliably and early;
- Companion diagnostics or biomarkers which deliver sensitive and specific results and;
3.Informatics or the analysis of large data sets collected from patients and/or a wider population.
The expectation is that the precision targeting approach will provide clinicians with the diagnostic tools and therapies to prescribe the “right treatment to the right patient while simultaneously reducing waste and yielding cost savings.” (2)
These cost-savings have not yet been realised across all disease areas. The reasons for this are multiple but relate chiefly to the fact that development costs are still being incurred. However, the system sounds biologically plausible when one considers the potential of fewer inappropriate investigations, reduced iatrogenic problems or unplanned admissions and improved potential outcomes for patients.
Breakthrough precision medicine
The second type of precision medicine, ‘breakthrough precision medicine’, derives from the development of fully personalised curative drugs; in particular, genetic and regenerative cell therapies, which it is anticipated will be tailored specifically to each patient’s genomics and disease features.
The key considerations in this category of innovation are the likely enormous costs of drug development against the therapeutic value for a patient who goes on to have a full and productive life.
Adding to the economic considerations, we should be aware of the influence of the burden of illness and the social impact involved in the potential of using a pooled national financial resource for expensive treatments for individuals with rare diseases.
This has been highlighted recently in the case of a dispute relating to the cost of a drug for cystic fibrosis. (3) This new therapy which is said to improve the lives of affected patients has fallen foul of NHS England pricing arrangements. Even though this is a conventional medication which has not yet reached the precision medicine category.
Additionally, in the UK we are nationally constrained by the NICE ‘value-based assessment’ of health technologies, which places a standard financial threshold on the incremental cost-effectiveness ration (ICER) per quality-adjusted life-year (QALY) of up to £30,000.
Having said this, NICE has revised their financial methodology for end of life technologies, where the ICER per QALY has been revised upwards to £50,000 and for very rare diseases, where the ICER per QALY has been increased to a £300,000 maximum. (4)
There have been criticisms of the NICE methodology, with researchers commenting that despite their transparent procedures it mitigates against expensive innovation and can result in ‘different values being placed on health gains for identical patients’ (5). Ultimately this may lead to a lack of access for patients who rely on the NHS. This could result in a situation where the much-touted democratisation of precision health, based on harvested population data, may end up benefitting only those with sufficient means to fund individual clinical trials, research and personal drug manufacture.
It is uncertain ‘how’ or indeed ‘if’ NICE will revise their value-based assessment approach to deal with these nascent technological advances that comprise precision medicine.
Conclusion
‘Precision targeting’ seems unarguable and feels like a direct continuation of the evidence-based medicine approach for all clinical practice. Over the next five to ten years it is likely that we will investigate and treat patients according to their defined genotype and phenotype.
‘Breakthrough precision medicine’ sounds tantalising to the patient and to the clinician. A ‘golden bullet’ approach to a disease entity unique to each patient seems to move us closer to a science fiction future of healthcare. But, just as this appears fantastical, the costs may also be fantastically out of reach for most patients.
As usual, science is moving faster than ethics. Our challenge, therefore, is to find a way to harness this new technology whilst retaining the benefits for even the most vulnerable in society.
References
- International Risk Governance Center Expert Workshop. The Economics of Precision Medicine Available from: https://irgc.epfl.ch/wp-content/uploads/2018/10/IRGC-2018.-The-economics-of-precision-medicine.-Workshop-report.pdf.
- Kogan et al. Delivering on the Value Proposition of Precision Medicine: The View from Healthcare Payers The American Journal of Managed Care Vol 24 No 4 177-179 Available from: https://pdfs.semanticscholar.org/45ae/baf56c76a5f1ff3ebdd34a6b6984790061b4.pdf.
- NHS and Vertex remain deadlocked over the price of cystic fibrosis drug BMJ 2019 364 Available from: https://www.bmj.com/content/364/bmj.l1094.
- Paulden M. Recent amendments to NICE’s value-based assessment of health technologies: implicitly inequitable? Expert Review of Pharmacoeconomics & Outcomes Research, 17:3, 239-242, 2017. DOI: 10.1080/14737167.2017.1330152.
- Paulden M et al Some inconsistencies in NICE’s consideration of social values. Pharmacoeconomics. 2014 Nov;32(11):1043-53. doi: 10.1007/s40273-014-0204-4 Available from: https://www.ncbi.nlm.nih.gov/pubmed/25145802?dopt=Abstract.
Contributor Details
Editor's Recommended Articles
-
Must Read >> From biobanking to precision medicine