Using artificial intelligence, scientists have tackled one of the toughest challenges in cancer research
The University of California San Diego School of Medicine scientists have used artificial intelligence to tackle one of the toughest challenges in cancer research: predicting when cancer will develop resistance to chemotherapy.
Chemotherapy treatment
All cells, including cancer cells, rely on a complex molecular machinery to replicate DNA during cell division. Most chemotherapy treatments disrupt this DNA replication process in rapidly dividing tumour cells.
However, predicting how a tumor will respond to these treatments has been a challenge due to the wide range of mutations within tumors.
Analysing genetic mutations
The machine learning algorithm analyses how genetic mutations collectively impact a tumor’s response to DNA replication-inhibiting drugs.
Testing their model on cervical cancer tumors, the team focused on cisplatin, a commonly used chemotherapy drug.
The model accurately predicted responses and identified tumors at the highest risk for treatment resistance. It also pinpointed the complex molecular machinery driving this resistance.
Trey Ideker, PhD, a professor in the Department of Medicine at UC San Diego School of Medicine, highlighted the significance of this achievement. “Artificial intelligence bridges that gap in our understanding, enabling us to analyse a complex array of thousands of mutations at once,” said Ideker. Unlike previous approaches that focused on isolated mutations, this algorithm considers the broader genetic landscape of the tumor.
DNA replication
The complexity of DNA replication, a target for many cancer drugs, has been a limitation in understanding how tumors respond to treatments.
Ideker explained, “Mutations in any one part of this system can change how the entire tumor responds to chemotherapy.” The researchers focused in on a standard set of 718 genes frequently used in clinical genetic testing for cancer classification.
Using mutations within these genes as input, the machine learning model was trained with publicly accessible drug response data, revealing 41 molecular assemblies where genetic alterations impact drug efficacy.
“Cancer is a network-based disease driven by many interconnected components, but previous machine learning models for predicting treatment resistance don’t always reflect this,” Ideker emphasised.
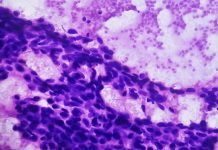
Cervical cancer
Instead of focusing on individual genes or proteins, the model evaluates broader biochemical networks crucial for cancer survival.
Putting their model to the test in cervical cancer, where approximately 35% of tumors persist after treatment, the researchers saw its accuracy in identifying susceptible tumors associated with improved patient outcomes.
The model also effectively flagged tumors likely to resist treatment, providing invaluable insights for clinicians.
Beyond its predictive capabilities, the model offered transparency in its decision-making process. Ideker emphasised the importance of this feature, saying, “Unraveling an AI model’s decision-making process is crucial, sometimes as important as the prediction itself.”
The transparency not only builds trust in the model but also identifies potential new targets for chemotherapy among the molecular assemblies the model has pinpointed.
This study marks a notable leap forward in the fight against cancer, offering a glimpse into a future where AI plays a key role in tailoring treatments to individual patients.