Professor Rhys Thomas & Professor Kevin Doughty from Virtual Ward Technologies, detail their plan for community health support via cutting edge virtual ward technology
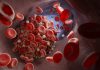
The evidence for supporting discharged patients at home, or closer to home, using virtual ward technology is well-established. The benefits are apparent to all stakeholders, as described in Table 1.
However, the focus has previously been on the columns towards the left of this table, i.e. on improving the performance and efficiency of NHS services.
The opportunities for supporting community and social care, and ultimately, self-care and communities, are also apparent and may be addressed by pivoting the use and type of technology from purely medical applications towards ‘virtual social care’.
Beyond these direct benefits relevant to patients who have been hospitalised for exacerbations of lung conditions, such as COPD, and cardiac or circulation issues, Virtual Ward Technologies offer interventions across the health and social care landscape.
Pre-habilitation before major surgery
The success of many surgical interventions can be improved by ensuring that patients are fit to undergo an invasive procedure.
Ideally, they could be offered personalised exercise and diet plans before being admitted to the hospital. Their health and fitness might then be tracked during their hospital stay, enabling a quicker and safer discharge using a conventional Virtual Ward technology arrangement.
Appropriate response to an emergency
The resources of ambulance trusts are being stretched to the point where they routinely fail to meet national emergency targets. Call handlers need to decide how to prioritise paramedic visits who, in turn, need to determine in a patient’s home whether they can be treated and left or taken to a hospital where they might end up on a trolley for several hours.
If vulnerable people had the technology available to them before an incident that could measure, record, and share vital signs data when appropriate, call handlers could use such information to accelerate response or to use community resources.
Similarly, if the patient must be left at home, changes in their functional status can be followed in real-time, allowing escalation procedures to be implemented.
Health & well-being improvement with technology
Strategies to improve general health often focus on the six Pillars of Prevention shown in Figure 1. However, success often depends on measuring key performance indicators such as body weight, resting heart rate (and variability) and sleep quality, but on recognising the issues and doing something about it.
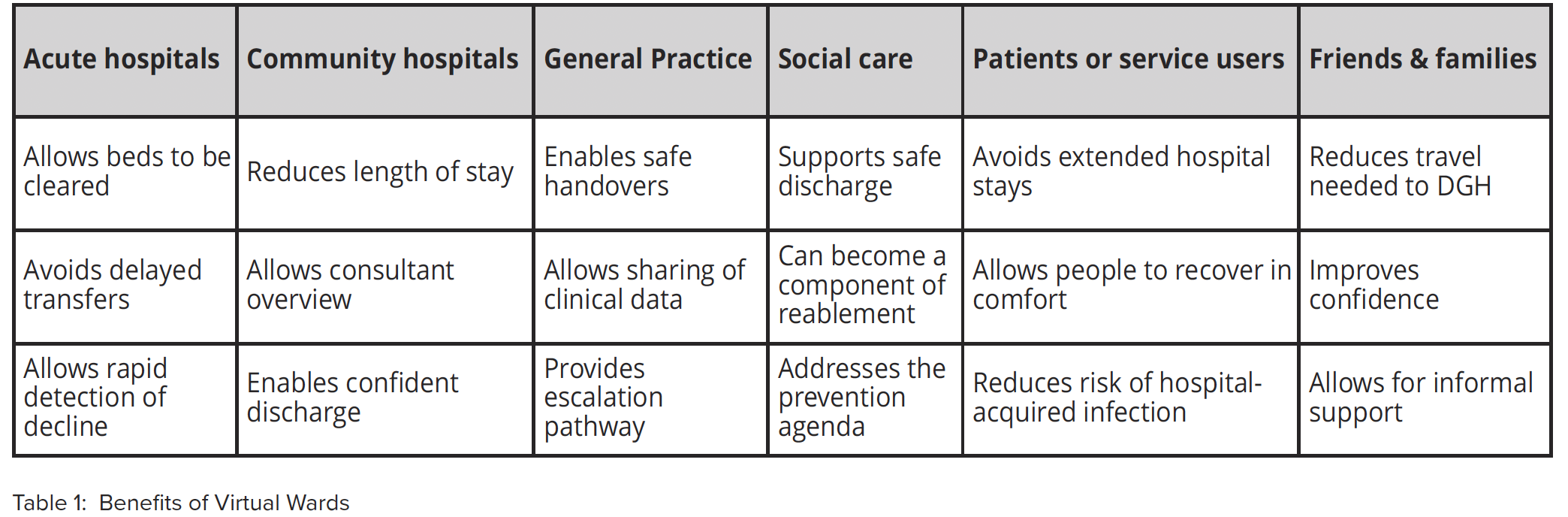
Virtual Ward Technology provides accurate measurements to clinical staff, but when used appropriately, it can provide feedback to the patient and their family. This enables the nudges and naggings necessary to change behaviour that can be far more effective than the advice of doctors, nurses and therapists in achieving the required compliance.
Introducing Virtual Ward Technologies at a population level
Introducing Virtual Ward Technologies at a population level is the key to all three examples described above.
This does not need the expensive and, therefore, limited medical devices that formed the original technologies provided in early work. Instead, it can benefit from the more recent developments in smart watches worn by the masses. With batteries that can last a week without the need to be recharged, they provide 24/7 provision of an increasing number of relevant parameters.
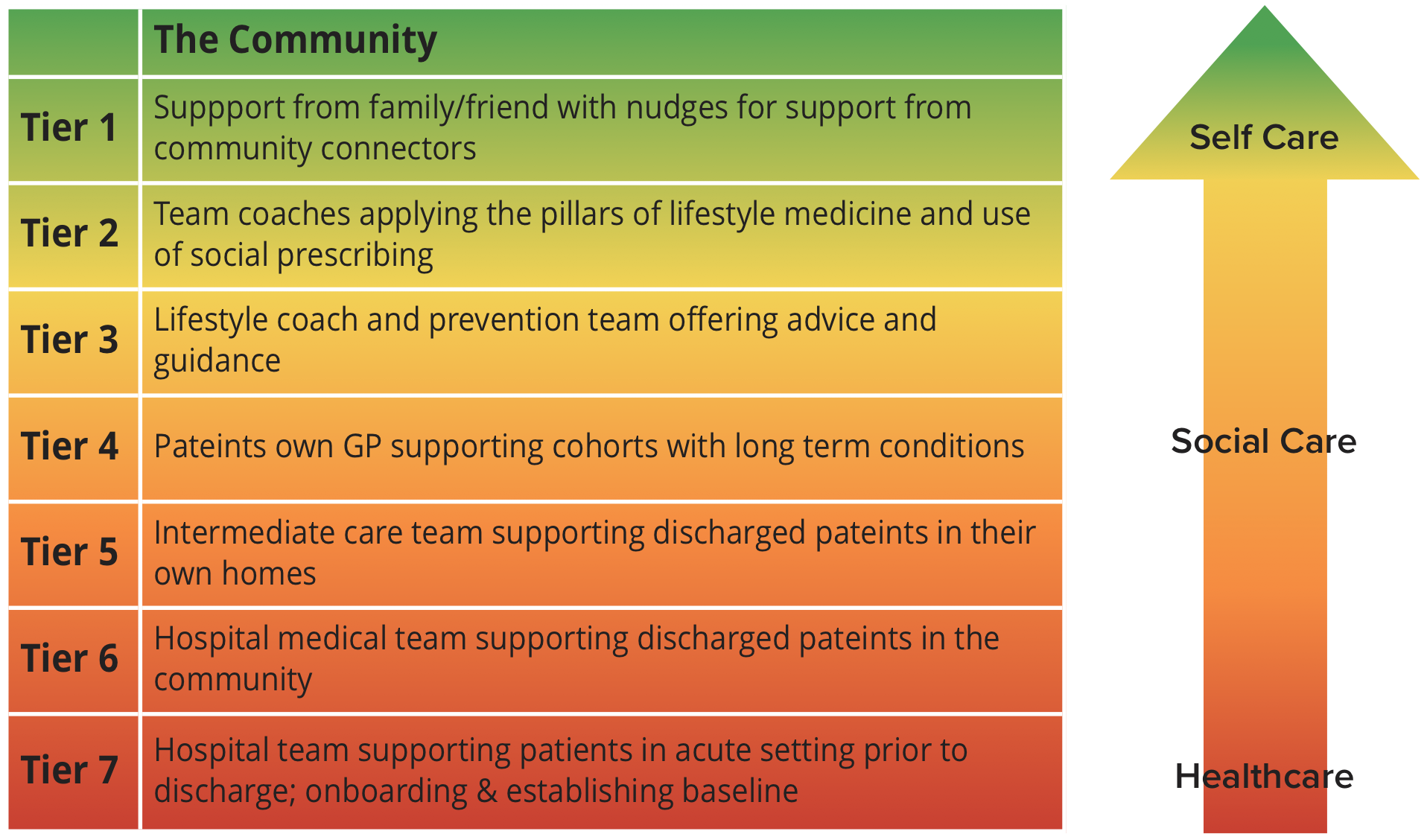
Virtual Ward Technologies have introduced a system of technologies whereby the whole family and community can support each other in health and wellness. The focus is then on the community and the social capital of individuals. This arrangement is at the heart of a new operational model shown in Figure 2.
This leverages the support of community connectors, first responders and, where appropriate,third-sector organisations, enabling low-level interventions, such as the introduction of assistive technologies, to be made early.
Combined with the power of data, this drives a prevention agenda that benefits society and makes health a personal responsibility, as it drives activity from acute healthcare setting back to the community and the individual and their friends and family.
Contributor Details
Editor's Recommended Articles
-
Must Read >> How virtual outpatient care can transform the NHS